| Rejection Criteria: |
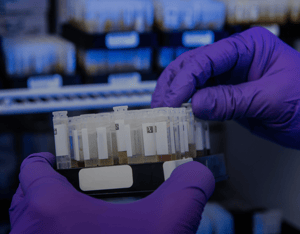
2.1 Sample Identification (Insurance): Sample identification is checked in the Set-Up Department. Each sample received is identified by a unique barcode number. This barcode number should be identical for all tubes received, except for the last two (2) digits which are container identifiers, and the barcoded slip ID. These are checked by the accessioning system which requires all tubes along with the slip ID to be scanned thereby verifying that the IDs match. All samples must be accompanied by a consent form (requisition). The consent has space for recording the client's name, birth date, sex, collection date, client signature, collector's signature, address, social security number, driver's license number, and policy number for other identifying factors. The insurance company on the consent dictates which tests are to be run on that sample. All discrepancies are referred to Customer Service for clarification before being processed. All procedures have a minimum sample requirement, along with any alternate acceptable samples (i.e., substituting plasma for serum). If the laboratory is unable to perform the assay due to insufficient sample volume to perform testing, it is reported as QNS (quantity not sufficient) or, if no sample is received, SNS (sample not submitted). Before a result of QNS, SNS or NSA is resulted for a test, every effort must be made to acquire an alternate sample to complete testing. The sample that is chosen must be of the proper matrix, must have been stored according to test stability requirements, must have sufficient volume and must not be needed for additional testing or client requested backup storage. 1. Sample or result is QNS, NSA or SNS for testing. 2. Technologist checks Sample Administration for an alternate aliquot of the same matrix or otherwise appropriate sample type. 3. If testing has been ordered on the chosen CID, the Technologist determines that all testing ordered on the alternate sample has been completed. 4. If no testing has been ordered on the chosen CID, the Technologist consults with the Laboratory Project Manager to determine that the sample may be used for testing. 5. The Technologist reviews the stability requirements of the test(s) and ensures that the chosen sample has been shipped, stored and handled in such a manner as to not compromise test results. 6. The Technologist acquires the specimen and ensures that it is of appropriate volume and that the degree of Hemolysis, Icterus, or Lipemia present in the specimen does not exceed known levels for interference. 7. The Technologist assures that the alternate specimen is delivered to the appropriate site or station for testing. If the test site is internal, the Technologist may alert the department personnel via email, that an appropriate, alternate specimen has been located. 2.4 Inappropriate Collection Tube or Procedure: Upon reviewing results, it becomes readily apparent which samples were collected and/or processed inappropriately. Refer to individual departmental procedures for the handling of these samples and the comments which are added. These results are usually entered as NSA, with a department appropriate comment code. 2.5 Hemolysis and Other Interferences: Each sample is examined for lipemia, hemolysis, and jaundice. This may be done by visual examination or run on the chemistry analyzer for determination of the serum indices. In addition, hematology samples should be examined for clots. The unsatisfactory sample is run, if possible, and appropriate comments are added according to department protocol. Note: This procedure does not infer that all “unsuitable” specimens are rejected or not analyzed. Some or all tests on a sample may not be analytically valid. In such cases the individual tests which are not affected may be reported. If a treating physician desires the result of an affected test the condition of the sample must be noted on the report. |