Recently Dr. Michael Fulks commented on 2020 mortality data from JAMA, citing an increase of 17.7% from 2019 to 2020 (click here for the full post). This week, Dr. Steven J. Rigatti comments on other recent articles discussing mortality, and how the finding may impact the insurance industry.
Two recent articles in the medical literature may provide some relevant insights for life insurers. One of these pertains to cancer screening tests and the other to a rural/urban disparity in mortality rates.
In the first article, published in JAMA, Schoenborn[i] et al. examined the mortality rates of individuals over age 65 who participated in the 2004 Health and Retirement Study. These data were linked to Medicare claims so that the individuals’ health care activities could be tracked. Two subpopulations were studied: 3,257 women eligible for breast cancer screening with mammography, and 2,085 men eligible for prostate cancer screening with prostate specific antigen (PSA) testing. Because this was a Medicare study, the mean age was higher (77.8 for women, 76.1 for men); follow-up was available for 10 years. Researchers were interested in determining if the choice to undergo screening was associated with an impact on the rate of mortality. To ascertain this, Cox models were used, controlling for a wide array of other variables relevant to mortality, specifically age, sex, comorbid illness, functional status, education, income, marital status, geographic region, cognition, self-reported health, self-care, and self-perceived mortality risk.
Results showed that those who undergo screening have lower mortality than those who do not. For women, undergoing mammogram was associated with a hazard ratio of 0.67, while for men undergoing PSA testing, it was 0.88 (both significant at the 95% level). This association was attenuated when a cognitive score was included, but not attenuated by the myriad other variables mentioned above.
Results showed that those who undergo screening [for breast cancer and prostate cancer] have lower mortality than those who do not.
This result is interesting because it does not consider the results of screening, merely the receipt of it. Somehow, the decision to undergo screening is itself a marker for improved mortality outcomes. It could be that this decision is a marker of healthcare sophistication and interest which winds up being protective. It should be noted that in the SEER cancer data, those early-stage screening-detected cancers like breast and prostate cancer have long been noted to be associated with lower mortality than an age/sex matched general population. This new research may help explain this somewhat mysterious phenomenon.
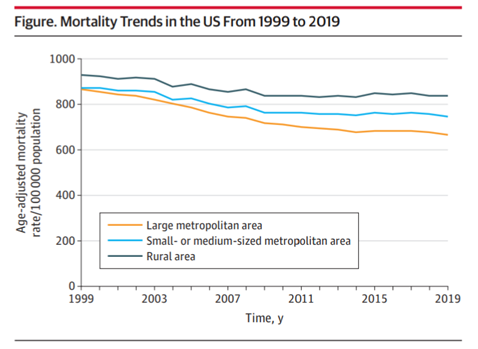
The second article of interest [ii] Medium article examines a trend in mortality during the pre-COVID years of 1999–2019, specifically a widening in the gap between rural and urban age-adjusted mortality rates. Cross et al. studied data from the CDC’s Wide-Ranging Online Data for Epidemiologic Research. They classified population density into large metropolitan (>1 million), small/medium metropolitan (50,000 to 1 million) and rural (<50,000). In all categories, the age-adjusted mortality rate declined over the two decades. However, the reduction was markedly smaller in rural areas (-0.5%, annual percentage change (APC)) vs. large metropolitan areas (-1.4% APC). When examined by age, the 25–64-year-old age group experienced an increase in mortality rates in rural areas (+0.6% APC), while the same age group in large metropolitan areas experienced a decrease (-0.9% APC). When narrowed further by race, rural non-Hispanic whites age 25–64 experienced a 0.8% annual increase, while non-Hispanic blacks, Hispanics and Asians all saw decreases (-0.9%, -0.7%, and -1.1%, respectively). These same young, rural whites experienced a 12.1% increase in mortality over the 20-year length of the study. The data does not contain individual variables as detailed as in the prior study, so isolation of cause of death or other confounders was not possible. This is especially unfortunate regarding income and education, which may be mediating the observed increase of the urban/rural disparity.
References
[i] Medium article Schoenborn NL, Sheehan OC, Roth DL, et al. Association Between Receipt of Cancer Screening and All-Cause Mortality in Older Adults. JAMA Network Open.2021;4(6):e2112062
[ii] Medium article Cross SH, Califf RM, Warraich HJ. Rural-Urban Disparity in Mortality in the US From 1999 to 2019. JAMA. 2021;325(22):2312.
About the Author
Dr. Steven J. Rigatti is a consulting medical director with Clinical Reference Laboratory, with 12 years’ experience in the life insurance industry. He is the current chair of the Mortality Committee of the American Academy of Life Insurance Medicine.